Interoperability & AIOps: Healthcare IT Priorities for 2026
Healthcare today runs on technology. Patient histories, lab results, imaging, billing workflows, clinical documentation, and even post-care follow-ups through mobile apps, all of it is powered by software.
As healthcare organizations move into 2026, many CIOs and IT leaders are stepping back to ask a critical question:
What must work better for us to scale care delivery without increasing risk or operational strain?
Across regions and care models, two priorities consistently rise to the top:
- Interoperability
- AIOps (Artificial Intelligence for IT Operations)
Not as buzzwords, but as foundational capabilities for modern healthcare systems.
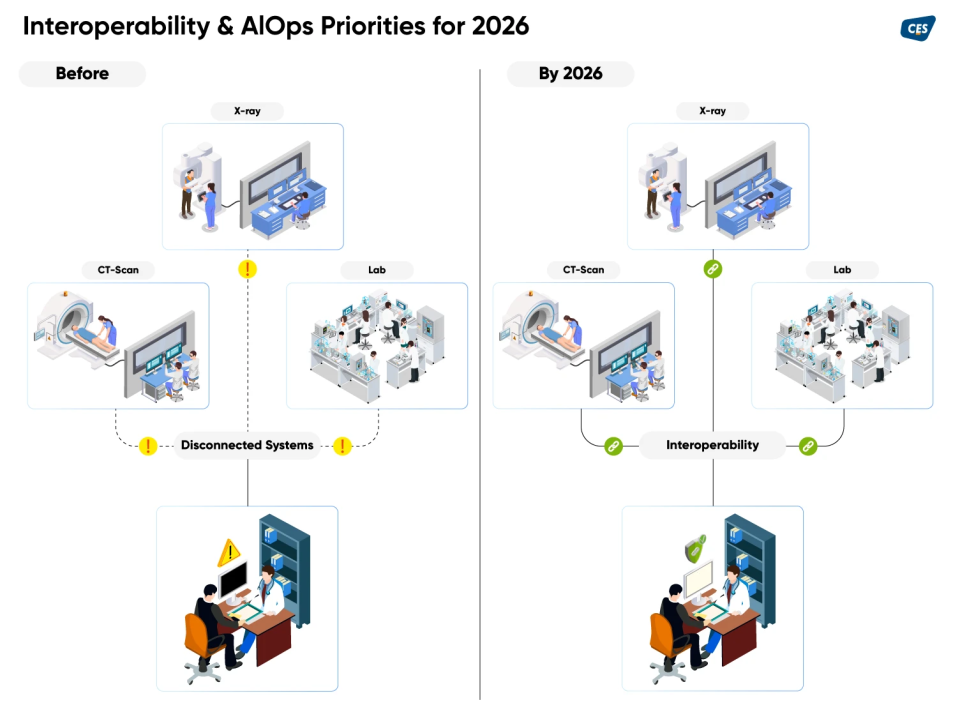
Interoperability in Healthcare: Beyond System Connectivity
Most healthcare organizations have already digitized their core systems.
What many underestimated was how difficult it would be to make those systems work together in real clinical and operational environments.
EHRs, laboratory systems, imaging platforms, revenue cycle tools, and care coordination applications often exist, but operate in silos. The result is fragmented data, manual workarounds, delayed decisions, and unnecessary administrative burden on clinical staff.
When interoperability works well, the impact is immediate and measurable:
- Reduced duplicate testing
- Faster access to complete patient records
- Lower administrative overhead
- Better-informed clinical decisions at the point of care
The Expanding Scope of Healthcare Interoperability
Interoperability is no longer limited to hospital systems alone.
Wearables, remote patient monitoring devices, digital therapeutics, and mobile health applications are generating continuous streams of patient data. Without consistent integration models, much of this data remains underutilized or worse, ignored.
This is where healthcare data standards play a critical role:
- HL7 & FHIR enable structured, API-driven clinical data exchange
- DICOM supports seamless medical imaging interoperability
These standards matter not because they’re trendy, but because they create a common language, making integration scalable, secure, and resilient instead of brittle and custom-built.
Regulatory Momentum Is Accelerating Interoperability
In the U.S., the TEFCA Common Agreement v2.0 now mandates FHIR-based exchange for participating health information networks. With facilitated FHIR workflows already underway and QHIN-to-QHIN FHIR pilots planned, interoperability is quickly becoming a compliance expectation, not an optional enhancement.
For healthcare leaders, this is a clear signal: API-first interoperability strategies are no longer future planning, they are current-state requirements.
Governance Is Now a Leadership Concern
As data flows more freely, governance becomes more complex.
Questions around data access, auditability, consent management, privacy controls, and cross-regional regulatory compliance can no longer be delegated entirely to backend teams. Secure data exchange is now a board-level topic especially as regulations vary across geographies and care models.
AIOps in Healthcare: From Reactive IT to Predictive Operations
While interoperability focuses on data movement, AIOps focuses on operational resilience.
Healthcare IT environments are increasingly hybrid and complex spanning on-prem systems, cloud platforms, medical devices, and third-party integrations. Traditional monitoring tools struggle to keep up, often reacting after issues impact clinical operations.
AIOps changes this model.
By continuously analyzing logs, metrics, events, and traces, AIOps platforms detect patterns early, correlate anomalies across systems, and enable teams to address issues before they disrupt care delivery.
Key Benefits of AIOps for Healthcare IT Teams
- Proactive issue detection for higher system availability
- Predictive capacity planning to manage infrastructure and cost
- Intelligent noise reduction to minimize alert fatigue
- Enhanced security visibility across hybrid environments
AIOps doesn’t replace IT teams, it augments them. It helps healthcare organizations stay resilient, efficient, and prepared for future growth without constantly operating in firefighting mode.
Cybersecurity & Resilience in a Highly Connected Care Ecosystem
Greater interoperability also increases the attack surface.
Healthcare organizations must align cybersecurity programs with regional and industry frameworks such as:
- HIPAA Security Rule (U.S.)
- NHS CAF-aligned DSPT (UK)
- DPDP obligations (India and emerging regions)
Modern healthcare architectures increasingly embed:
- Zero-trust access models
- Network segmentation
- Immutable backups
- Integrated SIEM and SOAR platforms
When paired with AIOps, these capabilities significantly reduce Mean Time to Detect (MTTD) and Mean Time to Respond (MTTR) critical metrics in environments where downtime directly impacts patient safety.
How CES Enables Interoperability and AIOps-Driven Healthcare Transformation
CES partners with healthcare organizations to modernize IT operations without disrupting patient care, delivering measurable improvements in efficiency, compliance, and outcomes.
Our Healthcare Capabilities Include:
- Seamless interoperability & system integration for accurate, real-time data exchange
- Cloud and infrastructure modernization for scalability, security, and cost optimization
- AIOps-driven automation for proactive monitoring and reduced downtime
- Data engineering & modernization to improve data quality and enable actionable insights
CES stands out through healthcare-focused delivery models, proven integration frameworks, and outcome-driven execution.
Real-World Impact Highlights:
- Improved care coordination using unified analytics for behavioral health
- Reduced diagnostic delays through zero-loss EHR-to-lab interoperability
- Faster lab turnaround times by automating clinical workflows
- HIPAA-compliant payer data ingestion with reduced manual errors
Looking Ahead: Interoperability and AIOps Are Foundational by 2026
In 2026, interoperability and AIOps are no longer optional upgrades. They will be core to how healthcare organizations operate, every day.
Those who understand their current maturity, invest with intention, and align technology with clinical reality will be far better positioned to:
- Support clinicians
- Protect patient data
- Scale care delivery sustainably
Next step:
Take an honest assessment of your interoperability and operational maturity. Then define a roadmap aligned with where healthcare IT is headed, not where it used to be.
Ready to accelerate your healthcare IT transformation? Talk to our healthcare technology experts: marketing@cesltd.com
